ADHD or Average, Rambunctious Child?
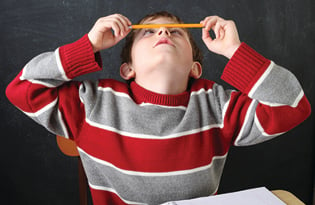
Walking into an exam room, I don’t hear the humming of lights or ticking of clocks, and I take little note of the man mowing the lawn outside the window or the nurse who just dropped a pen in the hallway — but my pediatric patient with Attention-Deficit/Hyperactivity Disorder (ADHD), the one squirming on the exam table, can’t help but notice. In fact, he has troubles answering my questions because so many distractions pull for his attention.
About 6.4 million children have received an ADHD diagnosis, according to data released by the Centers for Disease Control and Prevention, with boys being diagnosed more often than girls. In North Carolina, 15.6 percent of youth (ages 4 to 17) have been diagnosed with ADHD. The exciting news is after a thorough evaluation followed by appropriate medical treatment and accommodations at home and school, children with ADHD can thrive and be very successful.
ADHD is the most common neurobehavioral childhood disorder, and it’s one of the most studied medical conditions. Through research, we’ve learned that children with ADHD process information differently. That’s why children with ADHD, though usually very intelligent, constantly experience problems focusing, have trouble following directions, become easily bored or frustrated, appear “lazy” or “unmotivated,” tend to move constantly or fidget, and often act before thinking.
That list of symptoms sounds a lot like the average rambunctious child. That’s why diagnosing ADHD requires significant time, thorough information and professional experience. A diagnosis cannot be made in just a few minutes as part of a routine check-up. The American Psychiatric Association’s diagnostic manual provides 18 criteria for diagnosing ADHD, and patients must experience six of the nine inattention symptoms and/or six of nine hyperactivity symptoms to receive an ADHD diagnosis. Symptoms must commonly present themselves in two settings, like home and school, and show impairment.
Since it’s highly genetic, a methodical medical history must be gathered. It is also important to be sure these symptoms are not due to an underlying learning disability, mood issue (such as depression or anxiety) or environmental stressors. It’s crucial for physicians and families to take time during the diagnosis to identify the root issue.
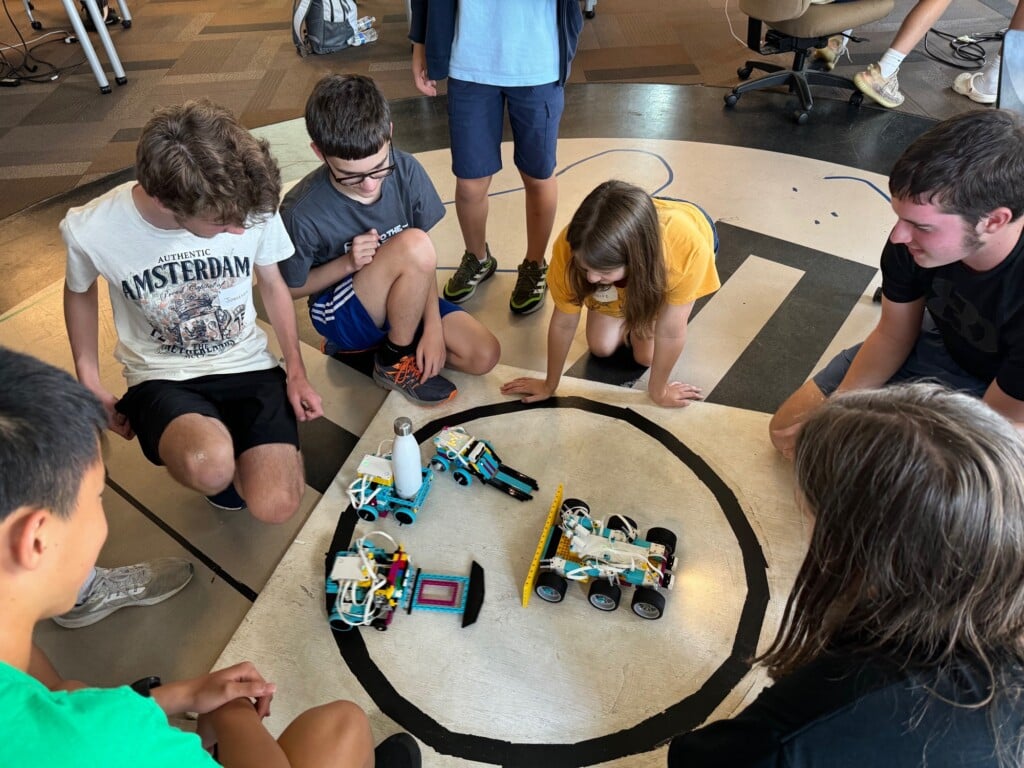
Once an ADHD diagnosis has been made, physicians can help parents develop personalized plans for children that may or may not include medication. Simple accommodations like providing kinesthetic breaks, strategically altering seating arrangements in the classroom, limiting homework time, providing visual prompts and removing environmental factors can make a significant impact.
If parents suspect ADHD, first schedule an appointment with your child’s primary care physician — and make sure it’s a separate appointment from the child’s routine wellness check. I also caution parents: Not all physicians are equally versed in diagnosis and management of ADHD or can take the lengthy time necessary to make a proper diagnosis. Sometimes it may be best to seek specialty care.
Barbara Kissam is a developmental pediatrician at Novant Health Developmental and Behavioral Pediatrics who has served as a specialist in ADHD and learning disabilities for the past 15 years.